National Healthcareer Association (NHA) | CBCS
What Is the 2013 NHA CBCS Certification?
Betty Jean is detail-oriented and pays attention to how the smallest details can affect the big picture. Her passion is to provide error-free curriculum to our teachers so they can spend time pursuing their own passions.
Editor's Note: This version of the NHA CBCS Exam will be retired in late 2021. Click here to learn about the updated version: What Is the NHA CBCS Exam (Updated for 2021)
As a health science curriculum developer, we work with thousands of teachers every year who need to prepare their students for industry certifications.
Many of these teachers are just starting their health science program and are deciding which certifications will give their students the most opportunity in their future careers.
One of the most popular exams that teachers consider is the NHA Certified Billing and Coding Specialist (CBCS) certification.
A medical billing and coding certification is sought-after due to the extensive career opportunities that it can open up to students post-qualification.
However, many teachers are not familiar with the concepts and skills necessary for a career in medical billing and coding and may need help developing a curriculum that will ensure students' success in the exam.
On this page, we’ll take a look into the 2013 version of the NHA CBCS certification and you’ll discover:
- What a medical billing and coding specialist does
- What career opportunities are available to students with the NHA CBCS certification
- What your students need to know to pass the NHA CBCS certification exam
- How you can prepare your students for the NHA CBCS certification exam
You’ll also have the opportunity to download our free NHA CBCS certification guide to learn how our digital health science curriculum can assist you with teaching your billing and coding lessons, and preparing your students for the certification.
What Is a Medical Billing and Coding Specialist?
The NHA CBCS exam is an industry certification developed by the National Heathcareer Association (NHA). It is designed to make sure medical professionals know how to properly code illnesses, procedures, and costs according to insurance standards.
According to the NHA, as a CBCS you may perform some or all of the following duties:
- Gather and review patient information
- Assign codes for diagnoses and procedures
- Verify documentation
- Submit claims reimbursements
- Prevent fraud
- Support coding and billing company-wide
- Educate health care providers
The skills learned through the NHA CBCS certification are essential to hospitals, physician offices, surgery centers, nursing homes, dental offices, home healthcare agencies, mental health facilities and even insurance companies and consulting firms.
Obtaining a billing and coding specialist certification will open up extensive opportunities for employment.
How is the 2013 NHA CBCS Exam Structured?
In order to be eligible to sit the NHA CBCS exam, students must be in possession of a high school diploma or GED equivalency as well as least one of the following:
- Successful completion of a training program in the medical coding and billing field in the past 5 years
- At least 1 year of supervised work in coding and billing in the past 3 years
The 2013 NHA CBCS exam consists of 100 questions (plus another 20 pre-test questions that are used to gather data).
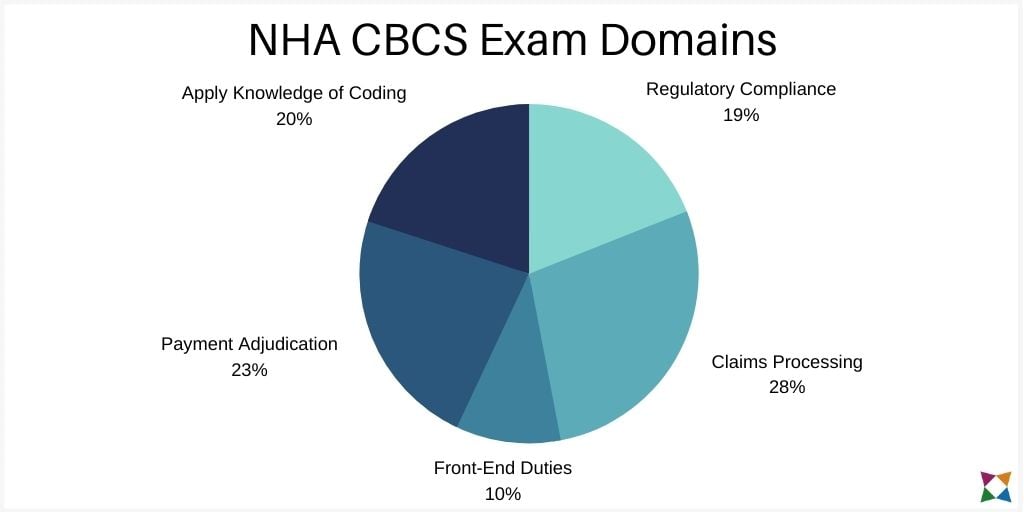
The questions fall into four topic areas, which the NHA refers to as ‘domains’.
- Regulatory compliance (19%)
- Claims processing (28%)
- Front-end duties (10%)
- Payment adjudication (23%)
- Apply knowledge of coding (20%)
Each domain is made up of different sub-topics that go into more detail of what your students are expected to know. Let’s dive into the details of each domain:
Domain 1 - Regulatory Compliance
The Regulatory Compliance domain has 19 scored items and is split into three sub-categories. Students will have to demonstrate that they can:
- Identify appropriate documentation required for release of patient information (6 scored items).
- Audit billing against medical documentation to prevent fraud and abuse (7 scored items).
- Identify major laws, regulations, and administrative agencies relevant to medical billing (6 scored items).
Domain 2 - Claims Processing
The Claims Processing domain has 28 scored items, split into two sub-categories. Students must be able to demonstrate that they can:
- Apply procedures for transmitting claims to third-party payers (14 scored items).
- Apply knowledge of the CMS-1500 form to accurately complete the appropriate fields (14 scored items).
This is the largest section of the exam, as it incorporates most of the day-to-day tasks that will be expected of students if they undertake a career as a billing and coding specialist.
Domain 3 - Front-End Duties
The Front-End Duties domain has 10 scored items and these are split into five sub-categories. Students must be able to:
- Ensure accurate collection of appropriate patient demographic and insurance information (2 scored items).
- Verify insurance eligibility to determine benefits (2 scored items).
- Compare and contrast government and private insurance (2 scored items).
- Process appropriate patient authorization and referral forms (2 scored items).
- Prior to the visit, determine appropriate balances due (2 scored items).
Domain 4 - Payment Adjudication
The Payment Adjudication domain has 23 scored items, across four sub-categories. Students must be able to demonstrate that they can:
- Analyze aging report (5 scored items)
- Post payment accurately (6 scored items)
- Interpret remittance advice to determine financial responsibility of patient and insurance company (6 scored items)
- Determine reason for insurance company denial (6 scored items)
Domain 5 - Apply Knowledge of Coding
Finally, the Apply Knowledge of Coding domain, has 20 scored items, and is split into two sub-categories. Students must be able to demonstrate that they can:
- Apply specific coding guidelines and conventions for diagnoses and procedures (10 scored items).
- Abstract the medical documentation by applying knowledge of medical terminology and anatomy and physiology (10 scored items).
For a rundown on the detailed tasks and questions that may appear under each of these sub-domains, download our NHA CBCS certification success guide.
How to Prepare Students for the NHA CBCS Certification Exam
There are many resources available to help you prepare your students for the CBCS exam, however they don’t help you teach your daily billing and coding lessons.
Developing a complete curriculum from scratch can be time-consuming and stressful for teachers.
In our experience, from working with teachers, it’s best to teach a base curriculum, then supplement this with test prep materials like study guides and practice tests
When implementing this type of blended approach, many teachers opt to use our HealthCenter21 digital curriculum as a supplementary resource.
HealthCenter21 has five modules that will help your students pass the CBCS exam:
Each of these modules aligns with one or more items listed on the NHA CBCS Test Plan.
You can download our NHA CBCS certification guide for an in-depth look at how each of these categories crossover with the domains included in the NHA CBCS exam, and how this will help you students prepare.


